

The Gilead Anti-Infectives Forum is a promotional website intended for healthcare professionals in the UK and Ireland, and has been designed, built, and funded by Gilead Sciences Ltd.
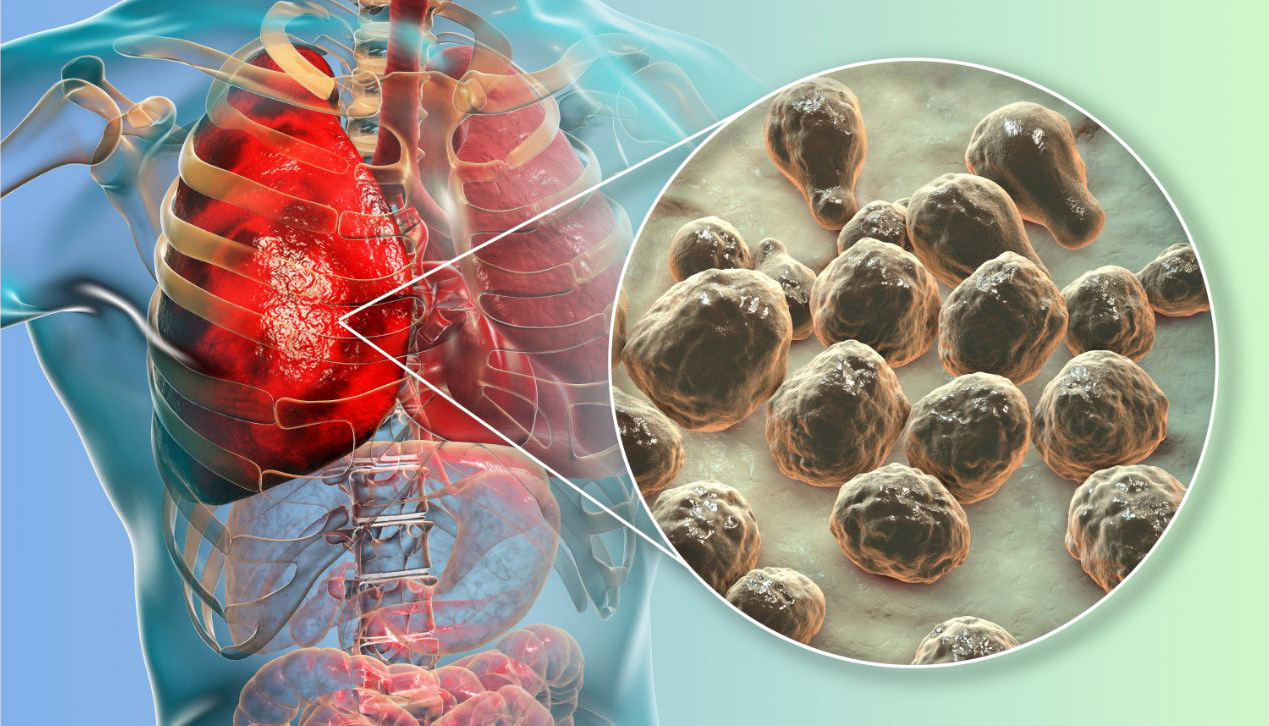
With the incidence of invasive fungal infections (IFIs) increasing globally in at-risk patients,5,6 identifying the signs, symptoms, and risk factors early could help you treat IFIs appropriately.1-3,7-11
Patients at risk of developing an IFI include those who have undergone transplantation (stem cell or solid organ), those prescribed targeted treatments for haematological malignancies and those living with advanced HIV.4-6,11-15 Please note that this list is not exhaustive.
 Uncontrolled diabetes16
Uncontrolled diabetes16
 Hospitalisation as a result of COVID-1917-19
Hospitalisation as a result of COVID-1917-19
 Nosocomial bacterial infection11
Nosocomial bacterial infection11
 Multiple organ failure20
Multiple organ failure20
 Major burns21
Major burns21
 Haematological malignancies11-14
Haematological malignancies11-14
 HIV/AIDS4,15
HIV/AIDS4,15

Major surgery (including intra-abdominal), organ transplantation, life support measures (including mechanical ventilation), total parenteral nutrition or insertion of medical devices (including shunts and catheters).11
Multiple invasive procedures and prolonged stay in ICU can also increase risk.11,22
 Immunosuppressants11
Immunosuppressants11
 Targeted therapies for haematological malignancies12-14
Targeted therapies for haematological malignancies12-14
 Corticosteroids and widespread use of broad-spectrum antibiotics11,23
Corticosteroids and widespread use of broad-spectrum antibiotics11,23
Increasing worldwide antifungal resistance may also contribute to the rising incidence of IFIs.11,24,25
A lack of definitive disease confirmation and access to timely fungal diagnostic test results can often lead to delayed antifungal treatment, increasing the risk of worse outcomes and mortality, compared to earlier treatment initiation.7,26
Early diagnosis and prompt treatment of IFIs in high-risk patients is key to ensuring favourable outcomes.6,7,13,26 Even in immunocompetent patients, if invasive pulmonary aspergillosis is not diagnosed and treated promptly, mortality rates can be higher than if IPA is diagnosed and treated promptly.27
In patients with invasive candidiasisa, mortality was high when antifungal therapy was delayed or inadequate and/or when source control was not quickly achieved.7,9,26
a. Invasive candidiasis includes three clinical conditions: candidaemia, deep-seated candidiasis and deep-seated candidiasis with associated candidaemia.59
The symptoms of an IFI can often be non-specific, making diagnosis difficult.28-30 Some of the more common clinical manifestations your patient may present with, include:28
 Fever
Fever
 Cough
Cough
 Dyspnoea
Dyspnoea
 Expectoration
Expectoration
When the diagnosis or fungal pathogen is unknown, treating eligible patients empirically may help to reduce mortality.9,39-41 Timely initiation of antifungal treatment has been shown to improve survival in some IFIs (e.g. candidiasis and mucormycosis)7,26,42,43
For a full list of indications please refer to the AmBisome Summary of Product Characteristics.
UK-AMB-0698 | November 2023